by Mary Imboden, PhD, HERO Membership Manager and Research Associate
 Mary Imboden is HERO’s membership manager and research associate. As a trained exercise physiologist, her background is in the benefits of physical activity on health and well-being. At HERO, she is interested in using her background knowledge to assess how healthy lifestyle behaviors, including physical activity can be effectively implemented into the workplace to improve health and wellbeing of all employees. Mary holds a Ph.D. in Human Bioenergetics with a primary focus on Clinical Exercise Physiology from Ball State University.
Mary Imboden is HERO’s membership manager and research associate. As a trained exercise physiologist, her background is in the benefits of physical activity on health and well-being. At HERO, she is interested in using her background knowledge to assess how healthy lifestyle behaviors, including physical activity can be effectively implemented into the workplace to improve health and wellbeing of all employees. Mary holds a Ph.D. in Human Bioenergetics with a primary focus on Clinical Exercise Physiology from Ball State University.
Health and well-being (HWB) initiatives have been introduced into the workplace over the past few decades. The goals: Improving overall health; reducing health-related costs; and increasing employee performance and productivity1. These initiatives have been implemented using different evidence-based designs2. Few studies have focused on the employer’s perceived effectiveness of an organization’s HWB initiative, even though it is well-established that perception and evaluation of worksite HWB initiatives are associated with participation and engagement3. As a result, perceived effectiveness could be indirectly associated with improvements in health and related costs. The HERO Health and Well-being Best Practices Scorecard in Collaboration with Mercer© (HERO Scorecard) includes questions on the perceived effectiveness of strategic planning, organizational and cultural support, participation strategies, programs, program integration, and measurement & evaluation to inform the development and implementation of effective HWB initiatives. The HERO Scorecard also assesses organizationally-reported impact on health risks and health plan cost.
Employer’s Perceived Effectiveness of Health and Well-being Initiative
In an attempt to capture employer perceptions about their organization’s HWB initiatives, the HERO Scorecard asks respondents how effective they believe their organization’s implementation of recommended practices is in each major domain assessed by the scorecard. Overall, a higher percentage of employers perceived their organization’s HWB initiatives as effective versus not effective. Specifically, 58% (n=964) of employers perceived the strategic planning for HWB in their organization as effective and 54% (n=970) of employers perceived their organizational and cultural support strategies as effective. When it came to programs and program integration, 61% (n=972) of employers perceived their HWB initiatives as effective in promoting a healthier workplace, and 42% (n=965) found the integration between their health-related vendors or programs as effective in contributing to the success of their HWB initiatives. When asked about participation strategies, 61% (n=964) of employers perceived their organization’s strategies as effective in encouraging program participation.
Impact on Participation, Health Risk, and Medical Cost
Overall, 41% of the 558 organizations providing these data reported that their initiatives were associated with significant (n=56) or slight (n=171) improvement in health risk. There were 560 organizations that provided information on medical cost trend and 29% reported a small (n=103) to substantial (n=60) positive impact on medical cost trend in association with their HWB initiatives. Only 11% that measured health risk and 14% that measured medical cost trend reported no improvement. However, 37% had not attempted to measure change in health risk and another 12% were not confident that their results were valid. A similar pattern was found for medical cost trend, where 45% of organizations had not attempted to measure the change in medical cost and 12% were not confident in the validity of their results.
Subsequent analysis examined the association between organizational reports of perceived effectiveness and three organizationally-reported outcomes including participation rates, health impact, and medical cost trend. Among the smaller sample of organizations that provided information on these outcomes, those that reported their HWB initiatives were effective had higher reported rates of health improvement and medical cost trend improvement. Details about how perceptions of effectiveness for the 6 areas of practice were related to these outcomes follow. Analyses for each section of the HERO Scorecard were limited to the number of organizations that provided responses to these optional questions and, as a result, sample size varied slightly for each analysis (168 to 237 organizations provided information on health improvement and 143 to 197 organizations provided data on medical cost improvement, depending on the analysis). Between 388 and 394 organizations provided data on health assessment participation and biometric screening, depending on the analysis. However, far fewer organizations (162 to 170 organizations depending on analysis) reported on coaching participation rates.
Strategic Planning
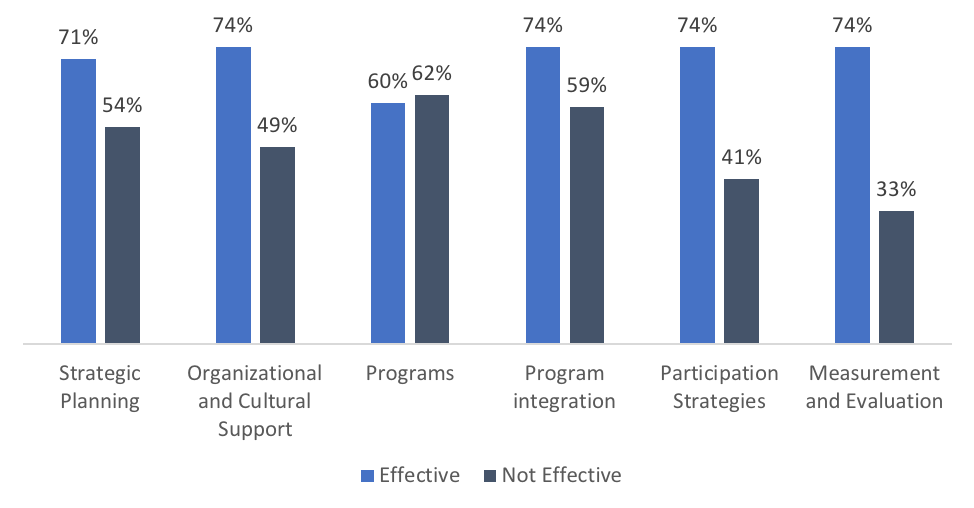
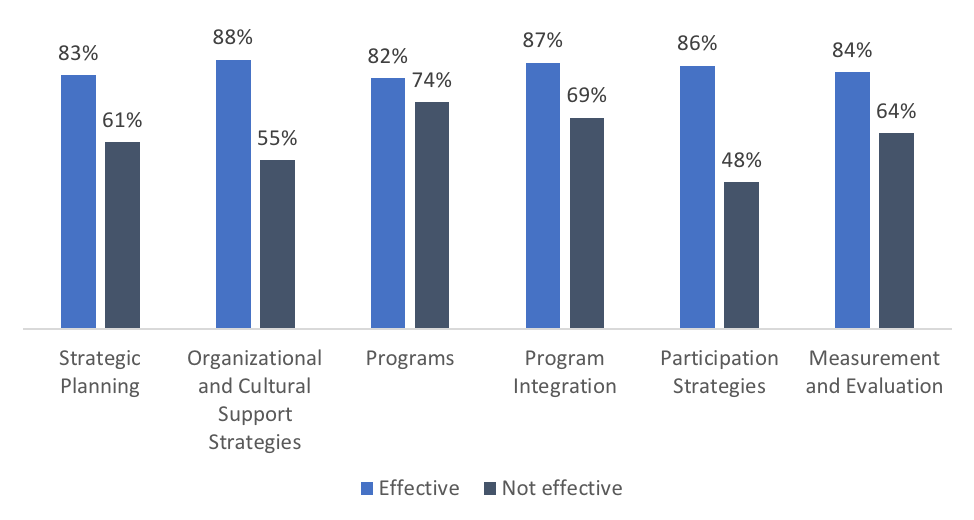
Organizations that perceived their strategic planning as effective had a much higher rate of reported health improvement (83% vs. 61%) and improvement in medical cost trend (71% vs. 54%) compared to those that did not find their strategic planning effective. Of the organizations that provided data, respondents that perceived their organization’s strategic planning as effective reported higher health assessment participation (53% vs. 44%) and biometric screening participation (52% vs. 43%) rates compared to respondents that perceived their strategic planning not effective. However, participation in health coaching did not vary depending on perceived strategic planning effectiveness.
Organizational and Cultural Support Strategies
Respondents that perceived their organizational support strategies as effective also had a higher prevalence of reported health improvement (88% vs. 55%) and improvement in medical cost trend (74% vs 49%) compared to those that perceived their organizational strategies as ineffective. Among the organizations that provided data, respondents that perceived their organizational strategies as effective reported higher participation in health assessments (52% vs 45%), biometric screening (51% vs. 45%), and health coaching (32% vs. 22%) compared to those that perceived their organizational strategies were not effective.
Programs
Employers that perceived their organization’s HWB initiatives as effective in supporting a healthier workforce reported a higher rate of health improvement (82% vs. 74%) and medical cost trend improvement (70% vs. 62%) compared with those that perceived their HWB initiatives were not effective. Employers that perceived their initiatives as effective in supporting a healthier workforce reported higher participation in HWB programs, including health assessment (51% vs. 47%), biometric screening (49% vs. 47%), and health coaching (30% vs. 26%) compared to those that perceived their initiatives were not effective.
Additionally, those that perceived their organizations HWB initiatives as effective in promoting a healthier workforce also reported a higher prevalence of health improvement (85% vs. 53%) and medical cost (74% vs. 41%) improvement. Among the organizations that provided data, those that perceived their initiatives as effective in promoting a healthier workforce reported higher participation in health assessment (53% vs. 43%), biometric screening (52% vs. 40%), and health coaching (30% vs. 25%) programs compared to those that perceived their initiatives were not effective in promoting a healthier workforce.
Program Integration
Similar to the patterns observed for the Programs section of the HERO Scorecard, respondents that perceived their program integration effective in contributing to the success of their HWB initiative reported a higher prevalence of health improvement (87% vs. 69%) and medical cost trend (74% vs. 59%) improvement than those that perceived their program integration was not effective. Respondents that perceived program integration as effective reported higher participation in health assessment (53% vs. 46%), and biometric screening (53% vs. 45%). No meaningful differences were found for participation rates in health coaching based on how organizations perceived the effectiveness of their program integration (29% vs. 28%).
Participation Strategies
Organizations that perceived their participation strategies were effective also reported higher prevalence of health improvement (86% vs. 48%) and medical cost trend (74% vs. 41%) improvement than those that found them not effective. Respondents that perceived their participation strategies were effective reported higher participation in health assessment (54% vs. 39%), biometric screening (53% vs. 37%), and health coaching (31% vs. 22%) programs compared to those that found their participation strategies ineffective.
Measurement and Evaluation
Respondents perceiving their data management and evaluation activities as effective had higher prevalence of health improvement (84% vs. 64%) and medical cost improvement (74% vs. 47%) compared to those that perceived these activities as not effective. Organizations perceiving their data management and evaluation activities as effective reported higher participation in health assessment (52 vs. 46%), biometric screening (54% vs. 41%), and health coaching (31% vs. 24%) compared to those that perceived their participation strategies were not effective.
Impact on Health Improvement Based on Perceived Effectiveness
Impact on Medical Cost Based on Perceived Effectiveness
Conclusion
- Organizations that perceived their organization as effective in strategic planning, organizational strategies, programs, program integration, participation strategies, and data management and evaluation reported higher rates of health and medical cost improvement.
- Organizations that perceived their organization’s HWB initiatives as effective in the six-domains assessed by the scorecard had higher rates of participation in health assessment, biometric screening, and health coaching in general. interventions, these results demonstrate the value of measuring and reporting on outcomes.
- Over half of respondents did not provide data on health improvements and medical cost. Employers should be encouraged to measure these outcomes to better understand the relationship between perceived effectiveness, participation, and health outcomes.
It has been reported that perceived effectiveness of HWB initiatives is associated with participation and engagement.3 The HERO Scorecard data supports this, as higher participation rates were reported for health assessments, biometric screenings, and coaching when employers perceived each of the six areas of practice assessed as effective. Whether perceived effectiveness of HWB initiatives has a direct association with health and medical cost improvement or an indirect association through the higher rates of participation, employers that perceived their organization as effective in strategic planning, organizational strategies, programs, program integration, participation strategies, and data management and evaluation reported higher rates of health and medical cost improvement.
The health and medical cost trend improvements in this analysis relied on employers’ responses on the HERO Scorecard. Because we do not know whether their responses were based on rigorous analysis of objectively-measured health, biometric, and medical claim data, these findings should be interpreted with caution. Despite this limitation, the results provide important information on the relationship between perceived effectiveness, participation, and health outcomes. This research may also help to inform future research on the relationship between perceived effectiveness and changes in health risks and medical costs.
This commentary is based on data from the HERO Scorecard Benchmark Database through June 30, 2018.
References
- Serxner S, Gold D, Meraz A, Gray A. Do Employee Health Management Programs Work? Am J Health Promot. 2009;23:1-12.
- Goetzel RZ, Henke RM, Tabrizi M, et al. Do Workplace Health Promotion (Wellness) Programs Work? Journal Occup Environ Med. 2014;56:927-934.
- Street TD, Lacey SJ. Employee Perceptions of Workplace Health Promotion Programs: Comparison of a Tailored, Semi-Tailored, and Standardized Approach. Int J Envir Res Public Health. 2018, 15, 881.
